Real Talk, Coach: How to Address & Manage Eating Disorders Among Your Baseball or Softball Players

Eating disorders are, unfortunately, very common among young athletes – which includes baseball and softball players.
Why is this particular population predisposed to having an eating disorder, and what can coaches do to address this issue head-on?
This article will cover what eating disorders are, common risk factors for eating disorders in athletes, and actionable prevention strategies.
Common Eating Disorders in Athletes
According to the American Psychiatric Association, eating disorders are “illnesses in which the people experience severe disturbances in their eating behaviors and related thoughts and emotions.”
At any given time, eating disorders affect several million people.
Most statistically often, these people are women between the ages of 12 and 35. But eating disorders can affect anyone at any age.
There are three main types of eating disorders.
These same disorders are also the most common ones found in athletics.
1. Anorexia
Anorexia nervosa is not maintaining a normal weight because a person either refuses to eat enough or exercises excessively. It’s characterized by limited food intake, problems with body image, or denial of low body weight.
Anorexia causes the body to go into starvation, resulting in a ceasing of menstruation, osteoporosis, mild anemia, severe constipation, and depression, amongst other symptoms.
2. Bulimia
Bulimia nervosa is characterized by episodes of binge eating and subsequent purging, either by inducing vomiting or taking laxatives.
During a binge, someone might consume thousands of calories and feel completely out of control while doing so.
People suffering from bulimia can be underweight, overweight, or at a normal weight for their height, so it’s more difficult to notice than anorexia.
There are some symptoms, however, including chronically inflamed throat, developing gastroesophageal reflux disorder, intestinal problems due to laxative abuse, or severe dehydration from purging fluids.
3. Binge-eating
Binge-eating disorder is recurrent episodes of binge eating, but without trying to purge directly after.
People who binge eat may still feel distressed and guilty about their binging episode and fast for several days or weeks afterward to compensate.
EDNOS
Not all disordered eating patterns fall neatly into these three categories, however.
They might be a mixture of anorexia and bulimia or even carry characteristics of all three.
These more challenging to categorize forms of disordered eating are called Eating Disorder not Otherwise Specified (EDNOS).

Why Are Eating Disorders So Prevalent in Sports?
Let’s start with the data.
Several studies and sports medicine researchers have shown that disordered eating is indeed prevalent in sports.
According to the National Association of Anorexia Nervosa and Associated Disorders, 13% of athletes in judged sports have eating disorders compared with 3% in refereed or umpired sports.
For reference, the lifetime prevalence of eating disorders in the total human population is 2.7%.
Which is still lower than the 3% average found in sports like baseball and softball. That extra .3% feels significant when the numbers refer to thousands of young ballplayers.
Here’s a couple more facts.
Eating disorders were more than twice as prevalent among females (3.8%) than males (1.5%).
And among athletes, eating disorders are most common in:
- Endurance sports
- Weight category sports
- Aesthetic sports.
But why are eating disorders more common in all sports than in the general population?
Experts have suggested several reasons, based on their research.
Firstly, as stated, it’s clear that eating disorders are most common in sports based on endurance, weight category, or aesthetics.
In endurance sports like long-distance running, lean body mass is associated with better performance. Endurance athletes will fixate on losing weight for physiological reasons.
And in sports where weight category determines your competition, such as boxing or judo, up to 70% of athletes may use dieting or disordered eating patterns to stay in their weight class just before a match.
Finally, in aesthetic sports such as gymnastics or diving, athletes are judged on appearance, particularly their ability to keep their body in a long, straight line as they fly through the air.
And all this research doesn’t even include a sport like bodybuilding, where judging appearances is the heart of the endeavor.
The various competition aspects of these sports make these athletes most susceptible to eating disorders.
But disordered eating affects many athletes in other sports, as well.
Professional and, more than ever, college athletes often receive media attention, with their games or matches televised, or their image appearing on magazine covers, banners, and merchandise.
With this kind of spotlight on them, research asserts that athletes can feel pressure to maintain a lean physique, at all costs.

Eating Disorders vs. Disordered Eating
What’s the real difference between eating disorders and disordered eating?
Thus far, we’ve used the two terms interchangeably, but they’re not quite the same thing.
People who have disordered eating symptoms might not necessarily have a formal, diagnosed eating disorder, but all eating disorders involve some form of disordered eating.
Many people suffer from disordered eating but don’t meet the narrow criteria for anorexia or bulimia. They may not even meet the requirements for an EDNOS diagnosis, either.
The term disordered eating developed along with the notion of the female athlete triad.
The female athlete triad is a syndrome in which female athletes suffer from three interrelated symptoms:
- Menstrual dysfunction
- Low energy availability
- Decreased bone mineral density.
According to the Academy of Nutrition and Dietetics, disordered eating describes a “range of irregular eating behaviors that may or may not warrant a diagnosis of a specific eating disorder.”

The NCAA’s Risk Factors for Eating Disorders and Disordered Eating
The National Collegiate Athletic Association (NCAA) recognizes that many of its college athletes struggle with eating disorders or disordered eating patterns.
The NCAA provides resources for coaches and athletes regarding disorders, including how to spot them and major risk factors.
According to Ron Thompson, a psychologist and consultant on eating disorders to the NCAA, there are four major risk factors that college athletes face concerning eating disorders:
- Prevalence: Women who participate in sports where a “lean” body is believed to provide a biomechanical advantage – long-distance running, gymnastics, diving, etc. – are the most at risk for eating disorders. Even more so than the men who also participate in these sports.
- Genetics: Studies show that genetics often account for predisposition to an eating disorder. Often, several members of one family will show signs of the same disorder.
A family member with an eating disorder doesn’t mean an individual is sure to develop an eating disorder, however. - Sociocultural factors: Societal and cultural pressures are often cited as the reason behind eating disorders in non-athletes. It’s easy to imagine that athletes feel influenced by these pressures regarding weight and appearance as well.
Many student-athletes may develop eating problems in response to stressors, such as being away from home and the demands of course work and sport participation. - Sport-related factors: Society puts pressure on people to look a certain way that often leads to an eating disorder, but so does the sporting environment.
Student-athletes might develop disordered eating patterns because they feel reducing body weight enhances their performance.
For some athletes, revealing uniforms – such as swimsuits for swimmers or spandex for volleyball players – are stressors that can lead to an eating disorder as well.
The sport-related risk factors above highlight an important issue when it comes to eating disorders – body image.

Athletes and Body Image Issues
Poor body image and dissatisfaction are predictive of disordered eating.
In a study of the risk factors and causes behind bulimia nervosa in adolescent girls, Stice, a researcher, found that the pressure to be thin or thin internalization produced dissatisfaction or a negative body image.
This negative body image may lead to changes in dieting and eating habits, which may then develop into bulimic symptoms.
Petrie and Greenleaf discuss the same effects, and associate internalization of body ideals, body dissatisfaction, dietary restraint, and bulimic symptoms with sociocultural and sport-specific pressures.
Reel and Voelker identify three major factors that influence negative body image in athletes specifically:
- Weight requirements: Sports teams that require certain weight limits, like cheerleading, might make participants think a body above or below the weight requirements is unacceptable.
In sports like wrestling, competitors chronically try to stay in one weight class or another by restricting dietary intake, leading to dehydration. - Uniforms: As I mentioned earlier, athletic uniforms lead to body image issues. The uniform is one of the most widely cited factors leading to pressure about body image.
Specifically, cheerleaders, swimmers, and dancers have reported experiencing negative body image and feelings of self-consciousness from their uniform – some dancers even considered it a distraction to their performance. - Pressure from teammates, coaches, and judges: Comments about changes in weight from fellow teammates and coaches can trigger body self-consciousness among athletes.
Many athletes are afraid of teammates and coaches noticing weight gain, and cite this as a top reason for feeling weight pressure.
The environment a coach creates may contribute to increased eating pathology among athletes as well. Low-support and high-conflict relationships between athletes and coaches could be a stressor that leads to disordered eating.
In sports with judges, such as gymnastics and figure skating, athletes may feel that appearance and weight are factors in their score. This pressure also contributes to negative body image.
Although a great deal of evidence supports the fact that female athletes are more at risk of eating disorders than male athletes, many male athletes feel pressures linked to body image and weight as well.
High-level male athletes might feel similar pressures from friends, family, teammates, and coaches, as well as from their sport’s weight requirements.
It’s also important to note that not all eating disorders among athletes are linked to negative body image.
In fact, some studies have found that athletes in endurance, weight class, and aesthetic sports have a more positive body image than non-athletes.
But Reel and Voelker suggest that although some athletes might have bodies that conform to socially and culturally accepted standards, they might still engage in unhealthy eating and weight control behaviors to improve athletic performance.
Negative body image should not, therefore, be the only predictive factor of an eating disorder that coaches, parents, and practitioners look for.

Health Consequences of Eating Disorders
Eating disorders take a serious toll on physical and psychological health.
Many athletes with disordered eating behaviors might construe their actions as “normal” and healthy within the sporting environment – where excessive training and dieting are sometimes perceived as part of being a good athlete.
What they don’t realize is that disordered eating patterns have detrimental consequences.
Physical health consequences
Purging behaviors are linked to electrolyte imbalances, dehydration, irregular heartbeats, and even heart failure. Other bulimic behaviors, like taking diuretic pills, can lead to kidney failure.
Anorexia can lead to premature osteoporosis, osteopenia, a drop in blood pressure, and the muscles – including the heart muscle – to waste away.
Other potential health consequences are peptic ulcers, pancreatitis, or gastric rupture.
Psychological health risks
Prolonged eating disorders or patterns are also associated with psychological health consequences.
Anorexia often occurs alongside depressive symptoms, obsessive-compulsive tendencies, personality disorders, substance abuse problems, and thoughts of suicide.
Bulimia is often associated with depressive symptoms, substance abuse problems, personality disorders, and anxiety.
Researchers have also identified behavioral and psychological tendencies specific to athletes with eating disorders:
- Secretive eating
- Avoiding eating situations, like team dinners, etc.
- Criticizing themselves for being fat when they are not
- Difficulty relaxing
- Resist seeking professional help
- Inflexibility to changing food or exercise regimens
- Exercising while injured
- Abnormal preoccupation with weight or shape. Either weighing excessively or refusing to weigh themselves at all
We’ll explore eating disorder detection for coaches and parents in just a bit, but this list of tendencies is a pretty good place to start.
The data below is about U.S. adults and isn’t specific to athletes, but it does speak to how often eating disorders overlap with mental disorders.
According to the National Institute of Mental Health, 56.2% of respondents with anorexia nervosa, 94.5% with bulimia nervosa, and 78.9% with binge eating disorder met criteria for at least one of the core DSM-IV mental disorders.

Famous Ballplayers Who Have Struggled with Eating Disorders
Athletes in team sports or so-called ball sports – like basketball, soccer, volleyball, football, baseball, softball – aren’t usually considered as high-risk for disordered eating.
Some research even shows that individual athletes might tend to be more weight and body-conscious than their counterparts in team sports.
But other studies have pointed to different evidence, which instead shows that the prevalence of eating disorders among team sport athletes has risen over time.
Baseball and softball players are, therefore, no exception.
And some elite ballplayers who struggled with eating disorders have been brave enough to share their stories publically.
Mike Marjama
Mike Marjama played for the Seattle Mariners in 2017 and 2018 before retiring. Two years ago, he revealed that he struggled with an eating disorder as a high school athlete.
In an interview with the National Eating Disorders Association, Marjama talked about trying to achieve a perfect “male physique” by limiting his calories and working out excessively.
His disordered eating patterns eventually turned into bulimia and by his sophomore year in high school, he had started an inpatient/outpatient and counseling program for his eating disorder.
He wanted to raise awareness about youth athletes and eating disorders, especially in boys and men. As a teenage boy suffering from an eating disorder, he felt that he didn’t have as many resources as teenage girls have.
For him, it’s important to end the stigma around men and eating disorders and realize that many men might be suffering from body image issues just as much as women and girls do.
Nancy Bowling
When University of Arizona softball pitcher Nancy Bowling took a leave of absence for the 2015 season, many wondered why.
The following year, when she came back to the team, she announced that she had sought treatment for an eating disorder.
In an interview with the Ventura County Star, she said that her anorexia had nearly destroyed her, and was fueled in part by her drive for perfection.
As an Arizona commit before her sophomore season of high school softball even started, she had a lot of eyes on her as an up-and-coming star.
So the pressure to be perfect and perform well started young for Bowling.
After getting treatment, she returned to the Arizona team with a much more balanced outlook on life, and was happy to be around her teammates again.
For these two examples of ballplayers who overcame their eating disorders, there are scores of others who still struggle.
Both Marjama’s and Bowling’s stories illustrate the importance of having a support network around you. As they both admitted that having a community, whether it was parents, friends, coaches, or teammates, helped them eventually develop healthier mindsets.
Preventing Eating Disorders Among Your Baseball or Softball Players
As a coach, what can you do to help prevent, identify, and address eating disorders amongst your ballplayers?
Prevention
To understand how to address eating disorders in ballplayers, it’s essential for coaches to be aware of the following risk factors:
- Individual genetic vulnerability
- Psychological vulnerability
- Sociocultural pressures related to food, body image, and diet
- Non-specific psychological stressors
- Revealing uniforms
- Sports environments that include weigh-ins or pressures about weight class
Coaches can create preventative strategies based on these risk factors by providing support to their athletes.
Support can be nutritional, which would involve helping athletes discover healthy diets. But this is only recommended for coaches with the proper educational and training backgrounds.
For the majority of coaches, this support should be more general, encouraging athletes to be their best selves rather than using harsh criticism and allowing inter-team bullying.
Coaches can also look to organizations such as UK Sport for helpful guidelines on avoiding eating disorders with their athletes.

Identifying Eating Disorders
As many sufferers of eating disorders hide their behaviors, identifying an eating disorder can be difficult.
There may be no apparent, outward signs in bulimia, for example, and distinguishing disordered eating from athletic eating isn’t easy either.
Athletic eating focuses more on what an athlete should consume to improve performance, whereas disordered eating emphasizes forbidding certain foods.
Using body mass index to detect an eating disorder among athletes isn’t reliable either. Muscular individuals will weigh more, but be leaner.
If a muscular athlete starts losing weight, there might not be a sign that it’s due to anorexia until the disorder has progressed considerably.
But coaches should still always be on the lookout for the tell-tale signs of an eating disorder:
- Anxiety or depression
- Excessive exercise habits
- Excessive restroom use
- Trouble concentrating
- Actively avoiding eating or eating situations
- Laxative or diet pill use
- Preoccupation with weight and eating, i.e claims of “feeling fat” despite being thin
Lastly, coaches can use screening programs and questionnaires to identify the presence of eating disorders among their athletes.
One of the most effective and simplest to administer to your ballplayers is called the SCOFF questionnaire.
It’s just 5 yes or no style questions – 1 point for each “yes” answer – that speak to the core features of both anorexia and bulimia.
If a player on your team scores greater than or equal to 2 points, then the presence of one of these eating disorders is likely. And you should consider taking further action.
Here’s the questionnaire below for you to use with your team.

How Baseball or Softball Coaches Can Take Action Against Eating Disorders
Once you suspect one of your ballplayers has an eating disorder, what should you do?
If you want to approach an athlete with an eating disorder, you should do so early, directly, supportively, and confidentially.
If you’re approaching them for the first time, and the issue seems serious, you'll likely want to enlist the help of a medical professional or psychiatrist, for an evaluation.
If the issue is more minor, you might be able to deal with it by offering nutritional resources and support, including devising a personalized nutritional strategy with help of a qualified nutritional expert.
Recovery and Rehabilitation
If a ballplayer has to sit out for a season to get treatment, they’ll usually be able to come back afterward.
Their reintegration to the team should mimic rehabilitation after an injury. Meaning start with a light training load at first with progressively more intense sessions.
Coaches should work closely with the designated therapist or physician, along with the athlete, to ensure a smooth recovery.
Good rehabilitation programs should include the following:
- Medical stability – bone density and electrolyte recovery
- Abstinence from disordered eating
- Consideration of the psychological stressors – that may have triggered the eating disorder in the first place
- Nutritional stability – nutrition should be sufficient to maintain weight with increased energy expenditure
In order for an athlete to recover and return to the team, there should be honest, open communication between the player, the coaches, and physicians or therapists.
One program that’s recently shown efficacy for serious athletes who are college-aged and up is the Walden GOALS Intensive Outpatient Eating Disorder Treatment Program.
This program was built specifically for adult athletes (18+) who need guidance on how best to optimize the balance between nutritional needs and performance goals.
But here’s the tenets of their program – which can be usual for athletes of all ages.

Final Thoughts on How Coaches Can Address and Manage Eat Disorders Among Ballplayers
As a coach, you have a responsibility to look out for the welfare of your players when it comes to athletic performance and overall well-being.
When a potential eating disorder is hindering your player’s success, both on the field and off, you can’t sit by and do nothing.
Get the facts about eating disorders and devise a strategy for dealing with them amongst your players. Don’t be afraid to bring the subject up and, above all, let your players know that you support them.
Wanna grow your baseball or softball coaching brand?
Get connected to new local and online lesson clients—along with all the tools you need to scale.
Download the free app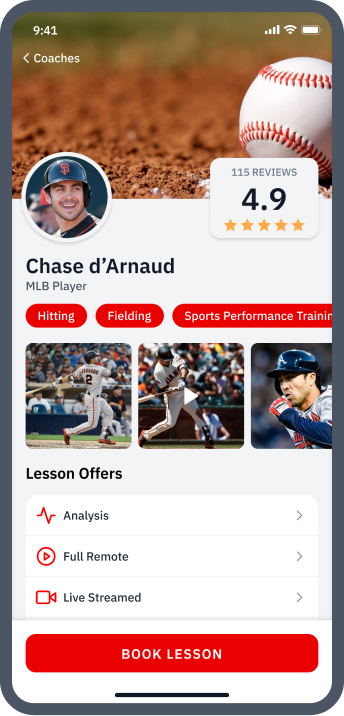

About the Authors
Dr. Hannah Whitney, DC
Doctor of Chiropractic at Uptown Whittier Center
Dr. Hannah Whitney is a practitioner at Sunny Hills Chiropractic Center and Uptown Wellness Center. She was also a 4-year college softball player at Alderson Broaddus University.
Courtney Withrow
Professional Writer
Originally from the U.S., Courtney is a Brussels-based freelance writer with a Master’s degree in International Relations. She grew up playing softball and still loves the game.
